7 Stages of Dementia Before Death
Dementia is a broad term for a decline in mental abilities that lasts a long time or doesn’t end. Symptoms include memory loss, trouble making decisions, and changes in behavior. 60%–80% of dementia cases have Alzheimer’s. Over 5 million Americans have Alzheimer’s, the 6th most significant cause of mortality in the US.
Alzheimer’s and other progressive dementias are incurable. Even though the disease gets worse over time and how long it takes can vary significantly from one patient to the next.
Changing personalities and dementia can make caring for a loved one difficult and uncomfortable. They might even forget who their closest friends and family are. Dementia requires excellent care and being a family caregiver, you must detect dementia patients’ dying signs. Hospice in this regard provides physical, emotional, and spiritual care to patients and their families wherever they live.
This article talks about the seven stages of dementia so that you know what to expect if you or a loved one have been diagnosed.
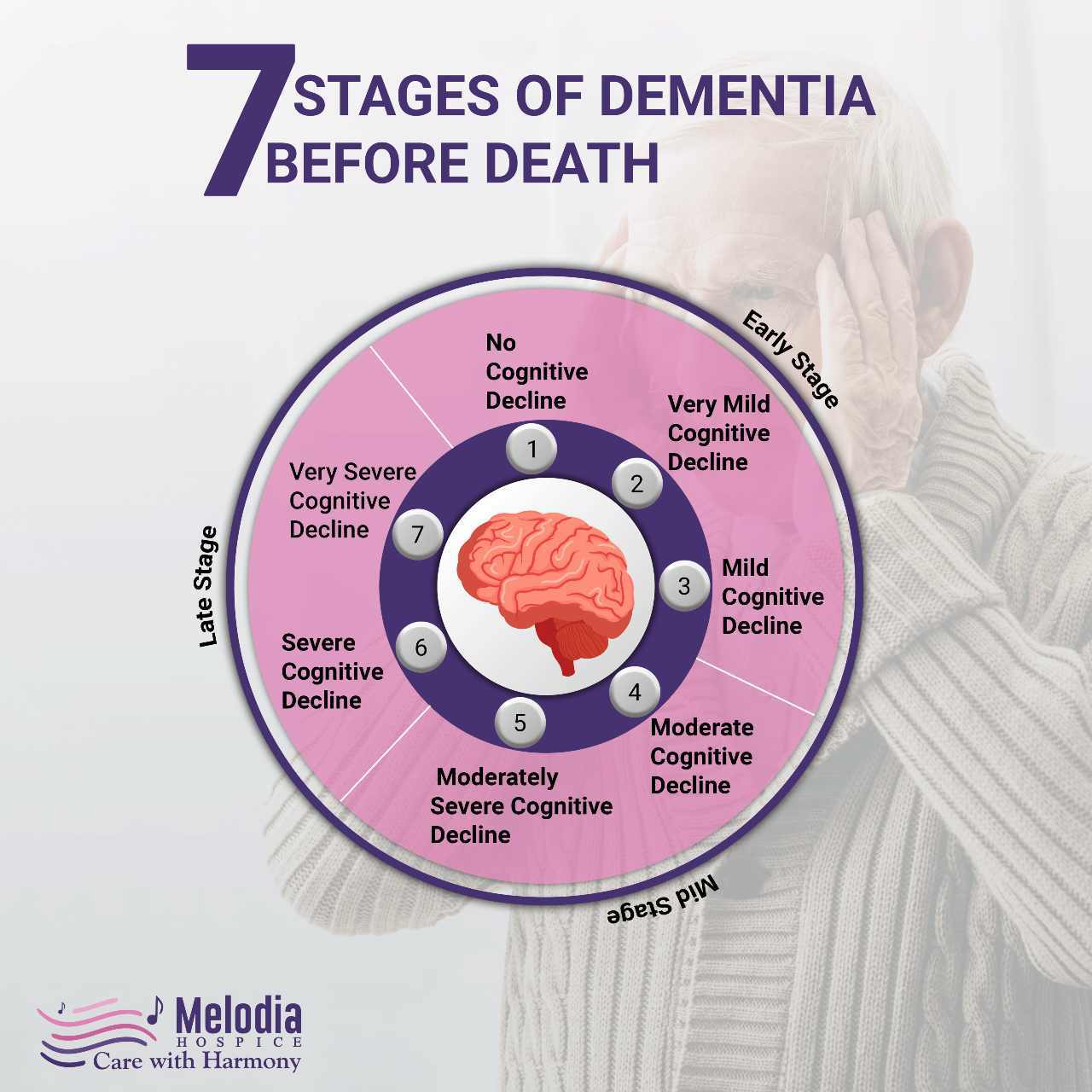
The stages are as follows:
- No cognitive decline
- Very mild cognitive decline
- Mild cognitive decline
- Moderatecognitive decline
- Moderately severe cognitive decline
- Severe cognitive decline
- Very severe cognitive decline
Stages 1–3 are pre-dementia; Stages 4–7 are dementia. Clinicians usually compare a person’s symptoms to the criteria mentioned for each stage and use their judgment to determine which stage the person is in.
The 7 Stages of Dementia
Below are the seven stages of dementia
Stage 1: No Cognitive Decline
The person has no memory loss, confusion, or cognitive impairment at this stage. However, as brain neurons die and lose connections, their structure and function may decline.
Stage 2: Very Mild Cognitive Decline
The person starts to have occasional memory gaps, such as:
- Misplacing everyday items
- Forgetting familiar names
Symptoms are unlikely to influence job or social interactions at this stage.
For instance, if the patient can pass memory tests during a clinical interview, the symptoms may be too minor to identify.
Stage 3: Mild Cognitive Decline
At this stage, cognitive impairment becomes apparent to the patient, friends, family, and colleagues.
Symptoms include:
- Walking or driving lost, especially in new places
- Reading and forgetting.
- Having trouble remembering the names of people they’ve just met
- Losing things of importance or value
- Problem-focusing and completing complex tasks
- Increasing social difficulties
- Forgetting words and family names often
- Poor work performance that colleagues notice
As the person’s symptoms become more apparent and get in the way of their ability to work, they may feel anxious.
Stage 4: Moderate Cognitive Decline
In this stage, a clinical interview will show a noticeable decline in the person’s mental abilities.
This stage may cause:
- Unawareness of recent events
- Trouble recalling the personal history
- Problems planning, traveling and managing expenses
At this point, the person will likely be able to remember the names and faces of loved ones and get around in familiar places. They may avoid stressful events to avoid anxiety and hide their distress.
Stage 5: Moderately Severe Cognitive Decline
From this stage on, the person may no longer be able to do things independently.
Symptoms include:
- Trouble remembering their address, phone number, or high school
- Confusion over the season, date, day of the week, or time.
- Difficulty counting backward from 20 by 2s or 40s by 4s (if educated and once able).
- Decision-making issues
The person may remember their names, their spouse’s, and their children’s, but not their grandchildren’s. They may need help with dressing but not eating or using the bathroom.
Stage 6: Severe Cognitive Decline
At this point, the person may need a lot of care because they are showing signs like:
- Trouble remembering their spouse, children, or primary carers
- Lack of awareness of all the recent events and situations in their life
- Trouble counting to 10 either backward or forwards
- Unawareness of time, location, and surrounds
- Unable to travel without assistance
- Wandering tendencies
The person may also go through changes in their feelings and personalities, such as:
- Paranoia, hallucinations, and delusions, such as talking to themselves or thinking that their caregivers want to hurt them
- Obsessive signs, such as cleaning something over and over
- Anxiety, irritability, and even dangerous behavior
- Loss of willpower because you can’t hold on to a thought long enough to finish the action.
The person may remember their name and discriminate between familiar and unfamiliar people during this period. They may need help with tasks of daily living, and they may have problems with incontinence and sleeping.
Stage 7: Very Severe Cognitive Decline
In the last stage, the brain loses contact with the body and can no longer tell it what to do.
The person may lose the ability to move and talk over time. They might only be able to make sounds or say things that can’t be understood. Eating, walking, and using the bathroom will require help.
Tips for Managing Dementia’s Final Signs
Caregivers must watch for signs of pain or discomfort in severe dementia patients, who typically have trouble communicating. Moreover, moaning, screaming, restlessness, grimacing, and sweating are some of the signs. Hospice or palliative care may also be needed to treat pain.
Hospice can provide a hospital bed or equipment to help end-stage dementia patients sit up.
Families struggle most when a dementia patient can no longer eat or drink. Dementia patients commonly try to remove feeding tubes or IV drips, causing discomfort and infection. Instead, make sure the person is relaxed. They can make their final transition in tranquility if they receive mouth care to prevent their mouths from drying out.
Helping Your Loved One
As a person with dementia gets worse, you can help them by being there for them in a loving and caring way. Seat them. Hold hands. Play their music.
Helping a loved one organize their company’s affairs is one of the best things you can do for them. Establish financial and healthcare powers of attorney to make decisions when your loved one cannot function. Look into funeral plans before you need them so you don’t have to make important choices in a crisis.
Talk to your loved one’s doctor about home palliative care and hospice care when they’re ready.
How Can Hospice Help With the Last Stages of Dementia?
Hospice care will ease caregiving’s physical and mental stress and help you spot dementia-related signs that indicate death. Nurses can update medicines and care treatments as needed. Aides can help with bathing, cleaning, and other personal care tasks. Social workers organize patient and family resources. Chaplains and bereavement specialists can assist with emotional and spiritual needs. Family members might also contact hospice without waiting for the doctor’s recommendation.
Melodia Care Hospice can benefit dementia patients and their families by providing information about hospice eligibility and scheduling consultations.


2 thoughts on “7 Stages of Dementia Before Death”
My motherinlaw Riana Bloem got demensia all zimers and Parkensons she don’t want to drink or eat she vomit she got terrible pain she sleep whole time of the day when she woke she just staar at one place can you help me please.
Sure we can. We understand it is difficult to see your loved ones struggling with dementia. Please contact us directly so that we can better understand her needs and explore how we can assist. You can also share your contact details and our representative will reach out to you directly.