End of Life Care
To say the least, talking about dying with a loved one is difficult. Being the health or social care professional in charge of discussing an end-of-life care plan with a dying or severely sick patient’s family members, on the other hand, is a tremendous professional difficulty.
It will be difficult – for everyone involved – but well-planned and executed end-of-life care will be extremely gratifying. Working with someone who is nearing the end of their life necessitates being knowledgeable, skilled, and empathetic. We’ll look at the following to assist you grasp what’s expected:
- Palliative care and end-of-life care
- What end-of-life care looks like?
- As a professional, be aware of the following principles.
- What to expect once a patient passes away
Palliative care and end-of-life care
It’s possible that these two concepts are interchangeable at times. Actually, there are various forms of care that require a variety of abilities and knowledge.
Palliative care
Palliative care aims to provide the best possible quality of life to those who are dying sooner than expected. It provides social support and attempts to restore a sense and daily functions. Working with someone who is towards the end of their life, on the other hand, is about making them as comfortable as possible while they die.
Palliative care is a type of care that provides support, care and treatment to those who are facing a terminal disease. You may have heard phrases like “life-threatening,” “terminal,” or “advanced” used in the same context. The following are some examples of life-threatening conditions:
- Cancer
- Chronic hepatitis is a type of liver disease
- Motor neuron disease (MND) is a type of neurodegenerative disease
Palliative care will address not only a person’s needs, but also their emotional, social and spiritual needs, with a focus on quality of life. Pain management is one of the first things that comes to mind, but social needs such as washing and dressing, as well as providing support to your patient’s family and friends, are equally crucial.
End of life care
Palliative care includes end-of-life care. Its goal is to make a person as comfortable as possible at the end of their life. Because we never know when someone will die, end-of-life care may be provided for weeks or even months. It’s usually given to someone who a doctor believes is in their final year of life.
End-of-life care, whether provided at home or in a facility, focuses on meeting physical and emotional requirements. It is critical to ensure that your patient is handled with decency and respect.
What End-Of-Life Care Looks like?
An End-of-Life Care is a plan that outlines the tasks that will be done by various experts as a patient approaches the end of his or her life. It refers to the efforts that must be performed to ensure that your patient is at ease in both their mind and body.
An End-of-Life Care is designed and implemented in six steps. If you’re working on one, here’s a quick rundown of everything you’ll need to do:
Step 1: Start a discussion about how to deal with a loved one’s death. You’ll have noticed that the patient is on the verge of dying away, and you’ll need to speak with them, their family, and their friends so that everyone is aware of what to expect and who will be making decisions.
Step 2: Assessment, planning, and evaluation – Recognize the patient’s wishes as well as his or her medical requirements. Take into account any cultural or religious requirements, as well as whether they prefer at-home care and anything else that is special to them.
Step 3: Care coordination — Each patient will have unique requirements. Plan ahead of time to have the right personnel on hand, such as nurses, care assistants, or doctors, who can fill in as needed.
Step 4: When the strategy is carried out, it is referred to as delivery. Care should be given wherever it is safest and as close to the patient’s wishes as possible, with consent always obtained.
Step 5: Final days – Get a sense of what death looks like so you can prepare for it. You can make a person’s final days comfortable rather than stressful if you know what to expect.
Step 6: After the patient has died, it is equally crucial to facilitate funeral desires and to support the patient’s loved ones in making decisions.
What are the principles of End-Of-Life Care?

Working on an end-of-life care plan necessitates familiarity with a few key concepts. These are the following:
- Individuality — there is no such thing as a one-size-fits-all approach to caring.
- Culture – a patient’s cultural, religious, and ethnic needs
- End-of-life care at home should always be a possibility.
- Contact must be sensitive and compassionate.
- Obtain the patient’s consent and if necessary, the consent of the individuals they have appointed.
- Professionals, patients and crucial people all require communication routes.
What are the signs of someone dying?
It takes time and practice to recognize a dying individual. Knowing how to recognize end-of-life indicators will help you prepare the patient and their loved ones for what is to come. You will grow more intuitive to your patients’ struggles with time, recognizing the signals like the back of your hand but understanding what to look out for in the beginning can be quite useful.
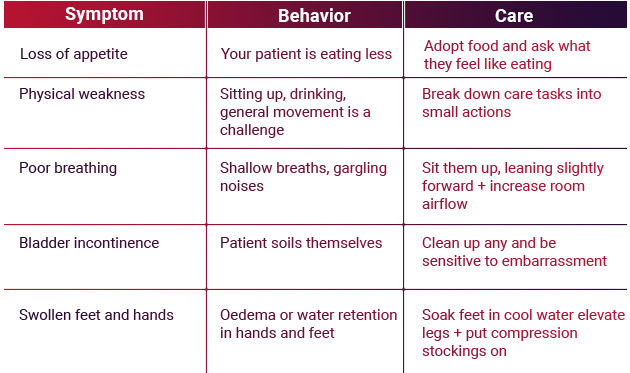
Here’s an overview of the five end-of-life symptoms and what you may do to ease the pain:
There is no way to truly “prepare” for a loved one’s death. However, knowing what signs and symptoms to look for at the end of a loved one’s life is one-way caretakers can start to prepare.
1. Loss of Appetite

Energy requirements decrease as the body closes down. Foods that are difficult to chew or digest, such as meat, may be rejected by your loved one. It’s typical for people to refuse meals or only eat a few bites. This can be a difficult period for the family emotionally. Our natural reaction is to suggest that our loved one eat, but this can be counterproductive near the end of life.
Near the very end
When people have trouble swallowing, they will begin to avoid beverages and food.
What you can do to help
- Modified (softer) foods that are easy to digest are available.
- Give your loved one extra time to eat and never rush them.
- Protein smoothies and other high-protein supplements are available.
- If beverages are being denied, try providing popsicles.
- To aid in comfort keep your loved one’s mouth and lips moist.
- Be patient and recognize that this is all part of the natural death and dying process, as difficult as it may be.
2. Physical Weakness

Simple activities such as sitting on the side of the bed, lifting one’s arms to change clothes and having a short conversation become difficult when food intake is reduced.
Near the very end
It may take a lot of effort for your loved one to drink from a straw, elevate her head or shift in bed. Movement may slow to the point where you must assist your loved one in making even the smallest of movements.
How you can help
- Recognize the need of energy conservation. Break up these duties into smaller intervals because your loved one will not be able to tolerate personal care for long amounts of time. Tasks should be scheduled in 15-minute increments.
- Prioritize keeping the person at ease over the task.
3. Poor Breathing

Most people begin to notice changes in their breathing as they get closer to the end of their lives. Air hunger is a term used to indicate shortness of breath. A terrified urge to breathe better is known as air hunger. The body is informing the heart and lungs that more oxygen is required, which can cause worry and anxiety.
Near the very end
Excessive secretions (moisture in the mouth and throat) can cause a loud gurgling sound known as the “death rattle” during breathing.
What you can do to help
- Understand that this is a normal part of the dying process, and your loved one will be unconscious of the changes in breathing at this stage.
- Consult your hospice nurse about medicinal patches that can help to dry up some secretions.
- Position your loved one in such a way that it takes less effort to breathe. Elevating the head or slightly sitting up with cushions and proper support are examples.
- Using a wet towel, moisturizer or lip balm, keep the lips and mouth moist.
- Suctioning the secretions is not recommended, according to your hospice nurse because it triggers a physiological response that causes the body to create more secretions.
4. Bladder incontinence (Changes in Urination)

Dehydration from reduced oral intake lowers blood pressure, resulting in reduced renal function (lower urine production) and finally, renal failure. Urine will darken, becoming brownish, reddish or tea-colored. Antibiotics will not be effective because it may have a strong odor that isn’t always caused by infection. Antibiotic therapy may hasten the loss of renal function in patients with significantly reduced renal function.
Near the very end
Urine and other waste materials build in the body as a result of kidney disease. As a result, mental acuity suffers even more. Your loved one will eventually enter a calm twilight or comatose state.
What you can do to help
New onset incontinence might be embarrassing if your loved one is still aware. It can also be difficult for family members, therefore aiding in the normalization of the situation and providing understanding and comfort is critical to your loved one’s care.
5. Swelling to Feet and Hands

As the disease progresses, edema and swelling of the feet and hands are caused by a variety of chronic disorders. Fluid is not being filtered and controlled adequately through the kidneys. Kidney function naturally declines as a person ages.
Near the very end
As your loved one approaches death, fluid in the lungs becomes more visible, causing shortness of breath. When you breathe you might hear a “rattle.”?
What you can do to help
- Position your loved one in a way that allows them to breathe more easily, for as by raising the head of the bed.
- Consult your hospice nurse about the benefits of using a compression hose on your legs. Elevate your loved one’s legs somewhat as well.
Caring for someone who is nearing the end of their life is difficult for everyone involved. Although no two deaths are the identical, you may still be prepared to provide the greatest possible support.
Individuals can get the care from MelodiaCare, they need in the location they prefer with end-of-life care and efficient communication. Allow us to assist you in caring for your loved ones by providing all of the support they require.
You can reach us at any time by contacting us through our 24/7 online customer support chat or by calling 1-888 635-6347 (MELODI-7) & Melodia Care Hospice.
